Obesity has become a global epidemic, affecting millions of individuals worldwide. While the association between obesity and cardiovascular diseases is widely acknowledged, evidence suggests a link between obesity and cancer. Researchers have been investigating the intricate relationship between these two conditions, shedding light on how excess body weight can influence the development and progression of various forms of cancer.
Multiple studies have established that obesity increases the risk of developing several types of cancer, including breast, colorectal, ovarian, pancreatic, liver, kidney, and esophageal cancers, among others. The reasons behind this association are multifaceted. Fat, or adipose tissue, produces hormones, such as insulin, estrogen, and adipokines, which can promote tumor growth and proliferation.
Additionally, chronic inflammation associated with obesity can create a favorable environment for cancer initiation and progression. Having a large amount of excess body fat puts stress on just about every bodily system. In the body, stress = inflammation.
Inflammation causes the production of chemicals that eliminate certain pathogens. These same chemicals damage DNA in the process, increasing cancer risk each time.
Obesity and the Body Mass Index
Obesity means one’s weight is higher than what’s considered healthy for their height and body composition. Doctors measure this using the body mass index (BMI). In adults, a healthy body mass index is between 18.5 and 24.9. Scores between 25 and 29.9 are labeled overweight. Scores over 30 are considered obese. There are a few problems with the body mass index and how it measures its scores.
Body builders, some of the fittest people by many standards, are often labeled obese by the BMI because their weight is above a “normal” range. The scale cannot distinguish between muscle, fat, and bone density. You can see how this highlights some limitations in the “holy grail” of how we measure healthy body weight.
The BMI also fails to measure fat distribution. People with abdominal obesity (they hold their fat around the torso) have a much higher risk of developing obesity associated cancers than those who carry their fat in the lower body. One’s risk of cancer is dependent on far more than a score on a scale with many issues, but it’s a good starting point.
Which Cancers Are Related to Obesity?
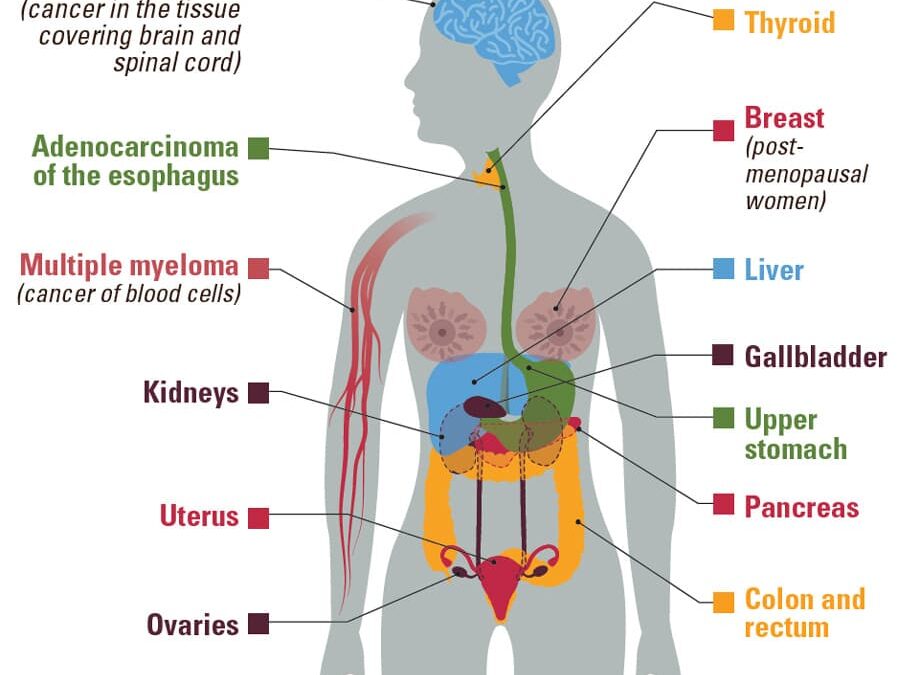
According to the CDC, being overweight or obese is linked with a higher risk of getting 13 kinds of cancer:
- Adenocarcinoma of the esophagus
- Post Menopausal Breast Cancer
- Colon and rectum
- Uterus
- Gallbladder cancer
- Upper stomach
- Kidney cancer
- Liver cancer
- Ovarian cancer
- Pancreatic cancer
- Thyroid
- Meningioma (a type of brain cancer)
- Multiple myeloma
- Prostate cancers
Other risk factors, such as, hormone levels, changes (called mutations) in genes, long-lasting infections, and tobacco and alcohol use can also contribute to these cancers. Excess body weight or obesity doesn’t mean that someone will definitely get cancer. But it does mean that there are more risk factors at play than if they kept a healthy weight.
Between 2005 and 2014, there was a noticeable trend in the United States where the incidence of most cancers linked to overweight and obesity increased, while the occurrence of cancers attributed to other factors declined. During this period, the rate of newly diagnosed cancers associated with overweight and obesity, except for colorectal cancer, witnessed a 7% increase. In contrast, the rate of cases related to factors unrelated to overweight and obesity experienced a drop of 13%. This demonstrates a relationship between obesity and cancer risk.
Explaining the obesity cancer correlation according to research studies…
1. Excess Fat Tissue and Cancer Risk:
Excess fat tissue acts as an active endocrine organ, releasing various hormones and signaling molecules that can disrupt the delicate balance within the body. Adipose tissue produces elevated levels of estrogen, insulin, and insulin-like growth factors, which have been implicated in cancer development. Breast, ovarian, endometrial cancer, prostate cancer, and colorectal cancers have all shown strong associations with obesity. Overweight and obese women have an increased cancer risk, likely due to these reasons.
To put it simply: Obesity can disrupt the hormone balance, making excess body fatness a major risk factor in reproductive cancers.
2. Chronic Inflammation and Cancer:
Obesity is characterized by a state of chronic inflammation, where fat cells release pro-inflammatory molecules. This sustained inflammation can contribute to the initiation and progression of cancer. Chronic inflammation can lead to oxidative stress and damage to DNA further increasing susceptibility to cancer. Inflammation-related cancers, such as liver, pancreatic, and esophageal cancers, have been linked to obesity.
To put it simply: Excessive weight gain puts detrimental stress on the body, increasing the risk of cancer over time.
3. Insulin Resistance and Cancer:
Obesity often leads to insulin resistance, a condition in which the body’s cells become less responsive to insulin. Insulin resistance increases insulin and glucose levels in the blood, creating a favorable environment for cancer cell growth. Obesity-related cancers, including postmenopausal breast cancer, prostate, and kidney cancers, have shown associations with insulin resistance.
To put it simply: Obesity can affect cancer risk by increasing the amount of insulin and glucose in the blood, making it more likely that cancer cells thrive.

Additional Hurdles: Cancer and Complications
Beyond its role in cancer, obesity can affect treatment outcomes and overall prognosis. Obese individuals often face challenges in cancer diagnosis and treatment, as excess weight can complicate imaging techniques and surgical procedures. Obesity increases the risk for diabetes and cardiovascular disease which can lead to impaired immunity and delayed wound healing, both of which play a significant role in someone being treated for cancer.
It’s not uncommon to hear doctors recommend their patients lose weight, especially as they get older. The complications of lugging around extra body weight put people at an increased risk of:
- Stroke
- Heart Disease
- Diabetes
- Arthritis
- Depression
- Sleep Disorders
So, what can I do now?
Given the strong link between obesity and cancer, preventive strategies play a crucial role. Encouraging a healthy lifestyle, including regular physical activity and a balanced diet, is key to weight management and reducing cancer risk. Avoiding tobacco use and keeping a healthy weight are two of the most important steps you can take to lower your risk of getting cancer. At Vivagen Health, our medical weight loss interventions can help you lose weight and provide you with a more balanced diet.
As research continues to unfold, it becomes increasingly evident that obesity and cancer are intertwined in complex ways. A healthy lifestyle, including regular physical activity and a balanced diet, is key to weight management and reducing cancer risk. By addressing the underlying factors linking obesity and cancer, we can help pave the way for effective interventions, early detection, and a longer, healthier life. Let us strive for a healthier future!
Achieve a Healthy Weight with Vivagen Health
Our accomplished team of professionals is committed to providing unwavering support throughout your journey, crafting customized plans specifically designed to cater to your distinct requirements and aspirations. Additionally, explore our Healthline platform for inspiring content on sustaining a wholesome lifestyle.
With Vivagen Health, attaining enduring triumph in weight loss is within your grasp, empowering you to embrace your fullest potential. Let us help you get back to a healthy body weight! Take action now by reaching out to us and starting your transformative experience today!